Navigating Healthcare Deserts: A Comprehensive Look at the HPSA Map
Related Articles: Navigating Healthcare Deserts: A Comprehensive Look at the HPSA Map
Introduction
In this auspicious occasion, we are delighted to delve into the intriguing topic related to Navigating Healthcare Deserts: A Comprehensive Look at the HPSA Map. Let’s weave interesting information and offer fresh perspectives to the readers.
Table of Content
Navigating Healthcare Deserts: A Comprehensive Look at the HPSA Map
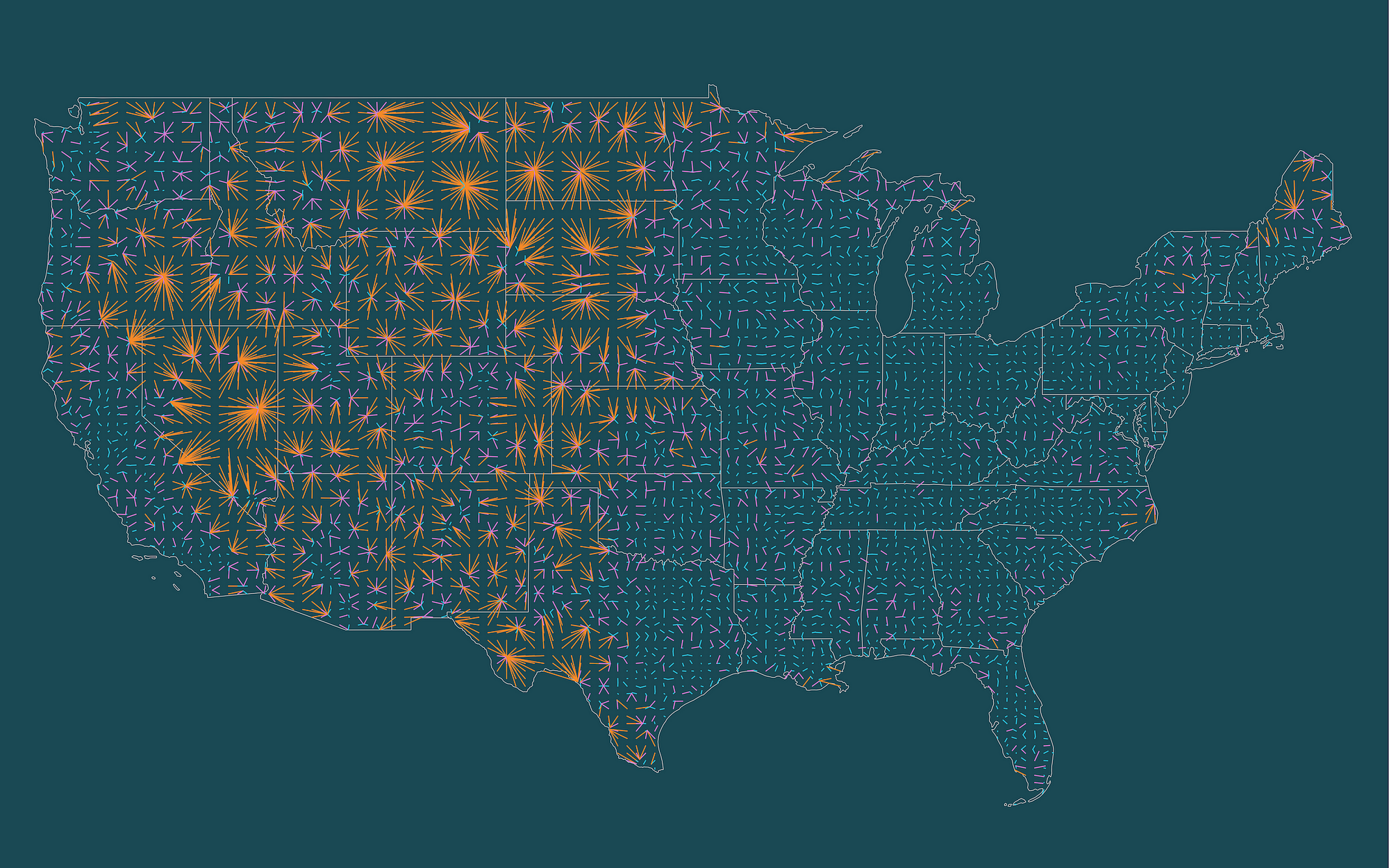
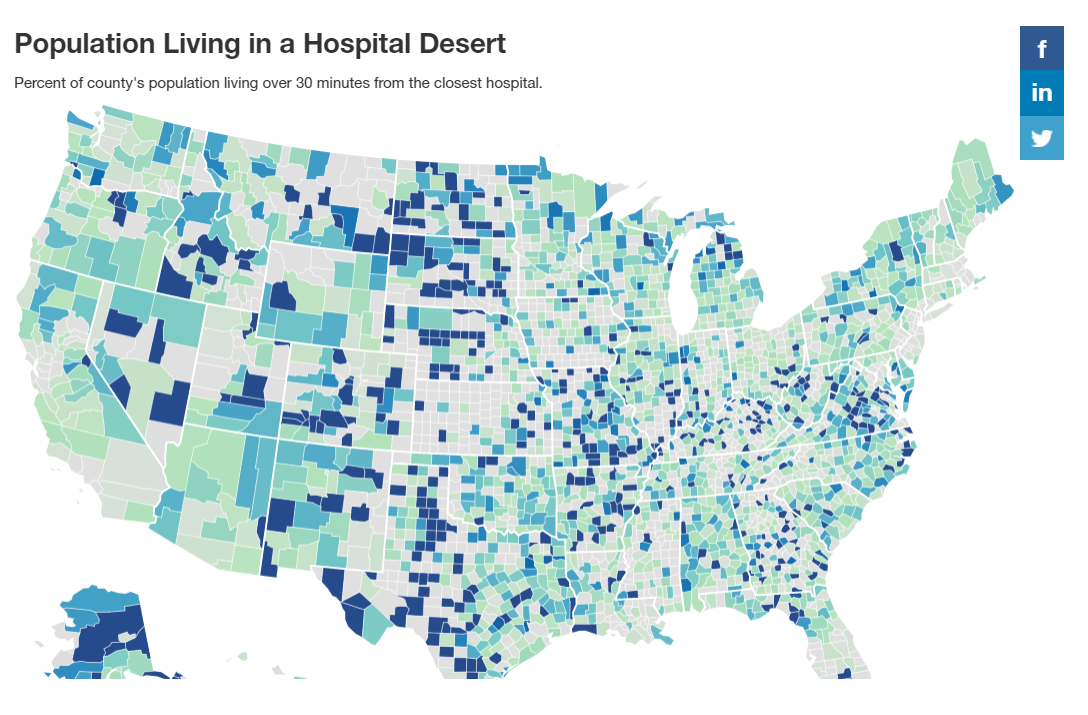
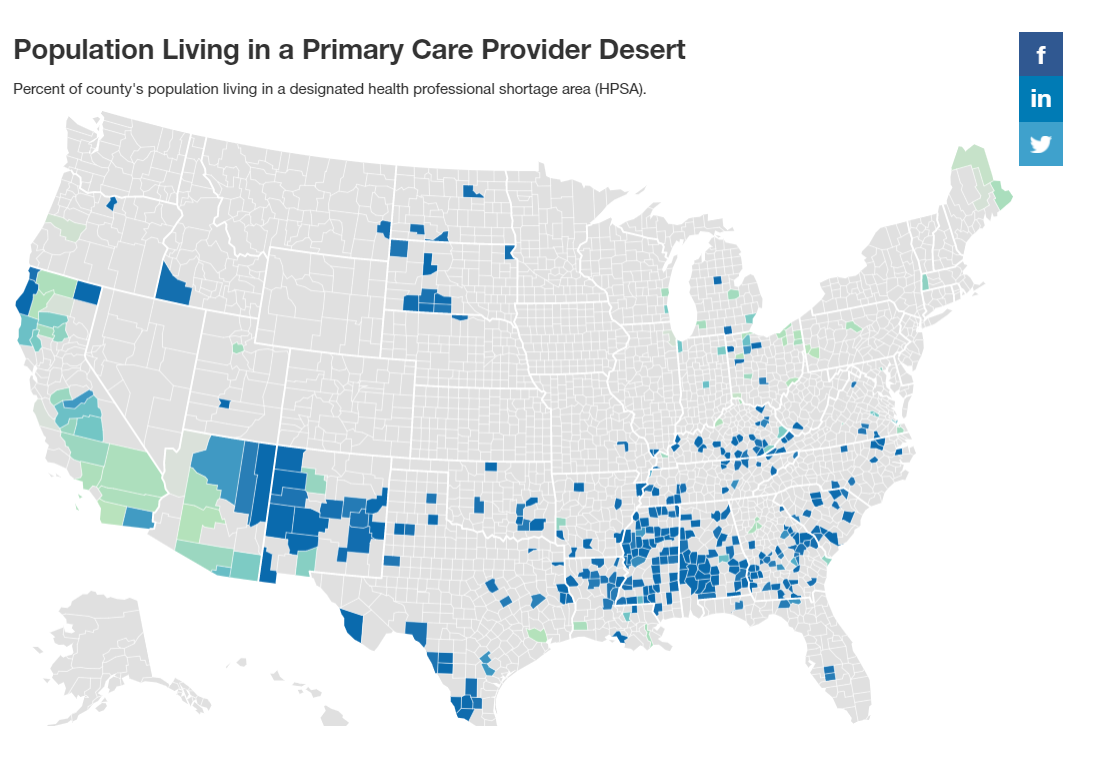
The distribution of healthcare resources across the United States is far from uniform. While some areas boast an abundance of medical professionals and facilities, others struggle to meet the basic healthcare needs of their residents. This disparity is starkly illustrated by the Health Professional Shortage Area (HPSA) map, a critical tool for understanding and addressing healthcare access challenges in the United States.
Understanding the HPSA Map: A Visual Representation of Healthcare Disparities
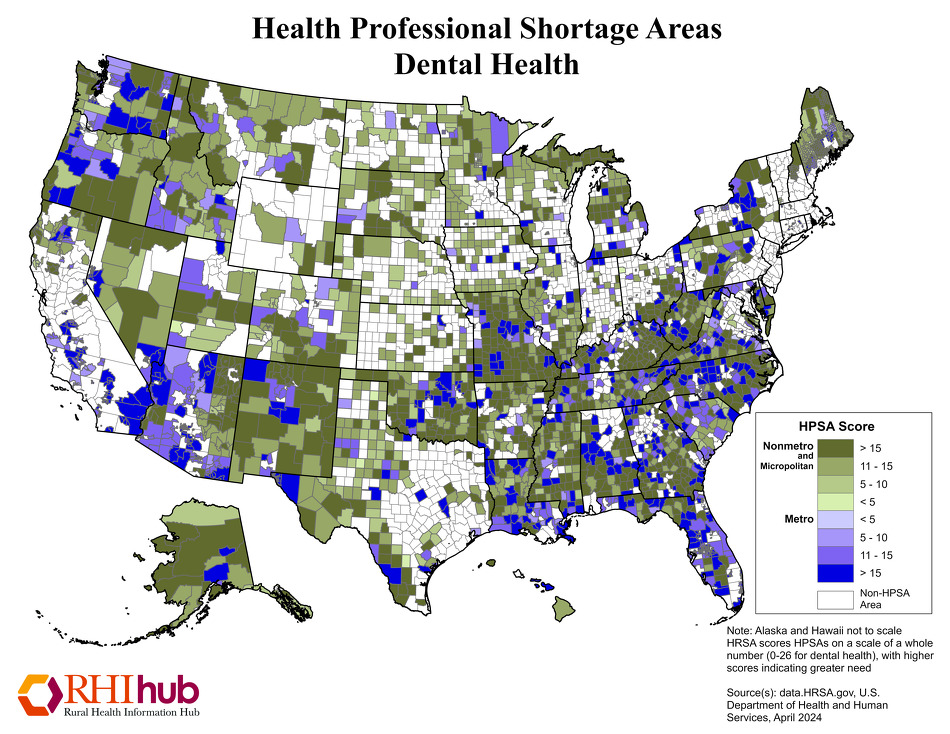
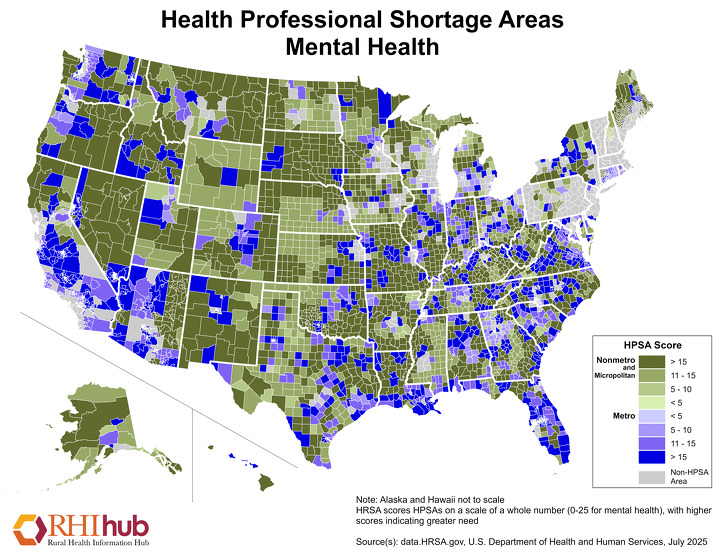
The HPSA map, developed and maintained by the Health Resources and Services Administration (HRSA), serves as a visual representation of areas across the country designated as having a shortage of healthcare professionals. This map is crucial for understanding the geographical distribution of healthcare resources, identifying areas with limited access to essential medical services, and guiding policy decisions aimed at improving healthcare access for underserved communities.
Categorizing Healthcare Shortages: A Multifaceted Approach
The HPSA map categorizes areas based on three primary factors:
- Population-to-Provider Ratio: This metric analyzes the ratio of residents to healthcare professionals within a specific geographic area. A high ratio indicates a shortage of providers relative to the population, highlighting areas where access to care is likely limited.
- Geographic Isolation: Remote or rural areas, often characterized by limited infrastructure and transportation challenges, are frequently designated as HPSAs due to their inherent difficulties in attracting and retaining healthcare professionals.
- Medical Need: Certain populations, such as those with chronic health conditions, disabilities, or specific medical needs, may require specialized healthcare services that are not readily available in their communities.
The Significance of the HPSA Map: A Guide for Policy and Action
The HPSA map plays a pivotal role in informing various aspects of healthcare policy and resource allocation. Its significance is evident in the following ways:
- Targeted Resource Allocation: The map serves as a critical tool for identifying areas in need of increased healthcare resources. By pinpointing HPSAs, policymakers can direct funding and support towards these communities to enhance healthcare access and improve health outcomes.
- Healthcare Workforce Development: The map helps guide programs aimed at training and recruiting healthcare professionals to underserved areas. By highlighting areas with a shortage of providers, these programs can focus their efforts on addressing specific needs and incentivizing healthcare professionals to work in HPSAs.
- Community Health Planning: The map empowers local communities to understand their healthcare needs and develop strategies for addressing them. By identifying HPSAs within their region, communities can work collaboratively with healthcare providers and policymakers to improve healthcare access and promote health equity.
- Research and Evaluation: The HPSA map provides valuable data for researchers and policymakers seeking to understand the factors contributing to healthcare disparities and evaluate the effectiveness of interventions aimed at addressing them.
FAQs: Addressing Common Questions about the HPSA Map
1. How is an area designated as an HPSA?
An area is designated as an HPSA based on a combination of factors, including population-to-provider ratio, geographic isolation, and medical need. The HRSA utilizes specific criteria and data sources to evaluate these factors and determine HPSA status.
2. What types of healthcare professionals are considered in HPSA designations?
The HPSA map considers a wide range of healthcare professionals, including physicians, dentists, nurses, pharmacists, and mental health professionals. Each category has its own specific criteria for designation.
3. What are the benefits of being designated as an HPSA?
HPSA designation opens up opportunities for communities to access various federal and state programs designed to improve healthcare access and address provider shortages. These programs may include loan repayment assistance, scholarships, and grants for healthcare facilities and providers.
4. How often is the HPSA map updated?
The HPSA map is updated annually to reflect changes in population, provider distribution, and healthcare needs. This ensures that the map remains a current and accurate representation of healthcare access across the country.
5. What are some of the challenges associated with HPSA designation?
While HPSA designation provides opportunities for resource allocation and program access, it also highlights the persistent challenges of healthcare disparities. These challenges include:
- Attracting and Retaining Healthcare Professionals: HPSAs often face difficulties in attracting and retaining healthcare professionals due to factors such as low salaries, limited resources, and isolation.
- Limited Infrastructure and Transportation: Remote and rural HPSAs may lack access to essential healthcare infrastructure, such as hospitals and clinics, and face transportation barriers that limit access to care.
- Social Determinants of Health: Factors such as poverty, lack of education, and limited access to healthy food contribute to health disparities in HPSAs, exacerbating the need for improved healthcare access.
Tips for Addressing Healthcare Shortages in HPSAs
- Invest in Healthcare Workforce Development: Support programs that train and recruit healthcare professionals, particularly those specializing in primary care and underserved populations.
- Promote Telehealth and Remote Care: Utilize telehealth technologies to expand access to healthcare services, particularly in geographically isolated areas.
- Enhance Infrastructure and Transportation: Improve access to healthcare facilities by investing in infrastructure development and transportation options.
- Address Social Determinants of Health: Implement programs that address factors such as poverty, education, and housing to improve overall health and reduce disparities.
- Foster Community Collaboration: Encourage partnerships between healthcare providers, community organizations, and policymakers to address healthcare needs and improve access to care.
Conclusion: A Call for Collective Action
The HPSA map serves as a powerful reminder of the persistent challenges of healthcare access and the need for sustained efforts to address these disparities. By understanding the factors contributing to healthcare shortages, leveraging the insights provided by the HPSA map, and implementing effective strategies, we can work towards ensuring that all Americans have access to the quality healthcare they deserve. This requires a collective effort from policymakers, healthcare providers, community organizations, and individuals alike. Only by working together can we bridge the gaps in healthcare access and build a healthier future for all.




Closure
Thus, we hope this article has provided valuable insights into Navigating Healthcare Deserts: A Comprehensive Look at the HPSA Map. We appreciate your attention to our article. See you in our next article!